Myasthenia Gravis: Symptoms, Causes, Diagnosis, and Treatment
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder characterized by weakness and rapid fatigue of voluntary muscles. The condition occurs due to the disruption of normal communication between nerves and muscles, which leads to muscle weakness. Understanding the symptoms, causes, types, and treatments of Myasthenia Gravis is essential for managing the disease and improving the quality of life for those affected.
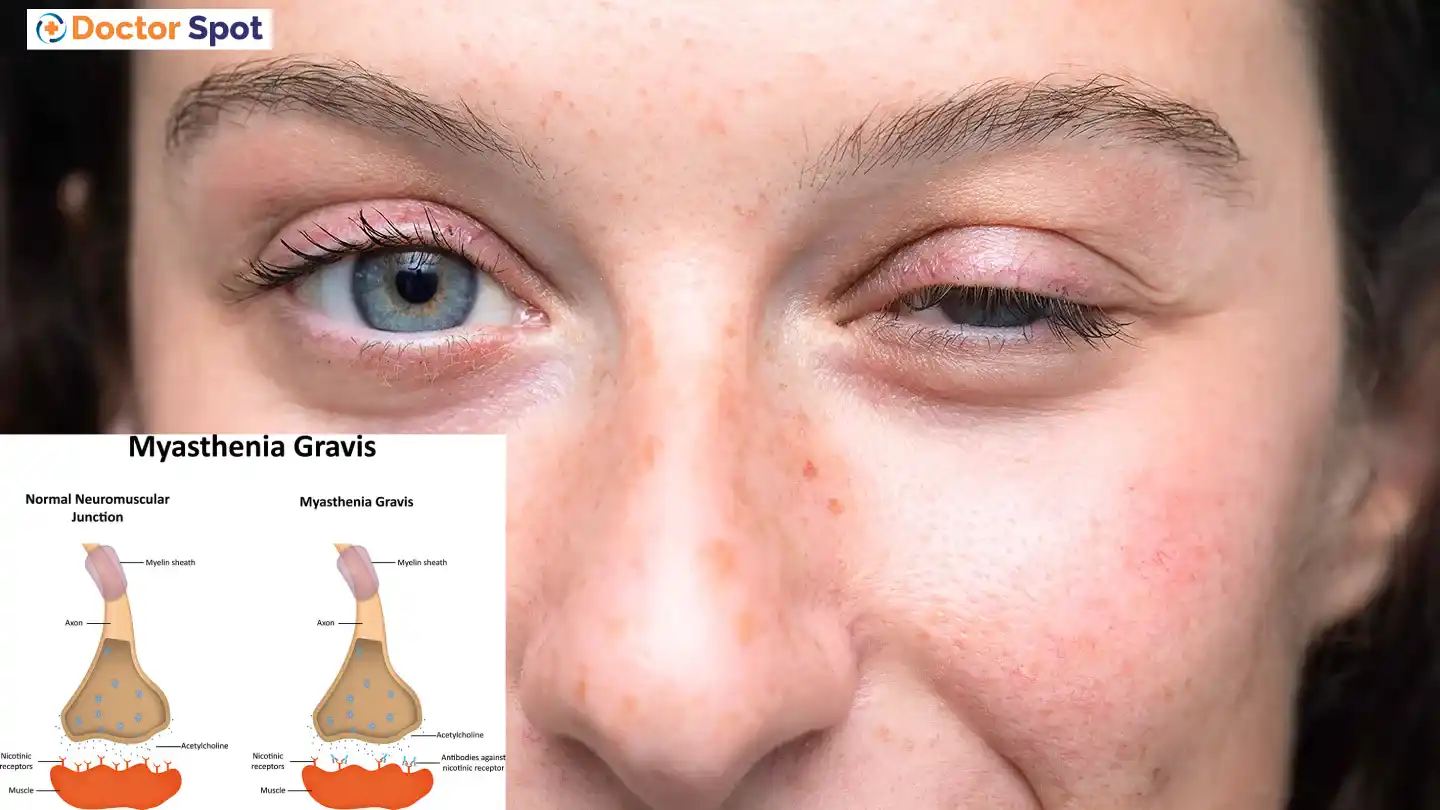
Symptoms of Myasthenia Gravis
The primary symptom of MG is muscle weakness that worsens with activity and improves with rest. The severity and specific muscles affected can vary greatly among individuals. Common symptoms include:
- Ocular Symptoms:
- Ptosis: Drooping of one or both eyelids.
- Diplopia: Double vision due to muscle weakness that affects the control of eye movements.
- Facial and Throat Symptoms:
- Dysphagia: Difficulty swallowing.
- Dysarthria: Slurred speech.
- Weakness in facial muscles: This can affect chewing and facial expressions.
- Limb and Trunk Symptoms:
- Weakness in arms, legs, and neck.
- Difficulty climbing stairs, lifting objects, or holding the head up.
- Respiratory Symptoms:
- In severe cases, MG can cause breathing difficulties due to weakness in the respiratory muscles, potentially leading to a myasthenic crisis, which is a medical emergency.
Causes of Myasthenia Gravis
Myasthenia Gravis is an autoimmune disorder, meaning the body’s immune system mistakenly attacks its tissues. The specific cause of this autoimmune response is not entirely understood, but several factors may contribute to its development:
- Antibodies: In MG, the immune system produces antibodies that block or destroy many of the muscle’s receptor sites for acetylcholine, a neurotransmitter crucial for muscle contraction. This prevents effective muscle contraction, leading to weakness.
- Thymus Gland: The thymus gland, part of the immune system, may play a role in MG. Abnormalities such as thymomas (tumors) are often found in patients with MG. The thymus is thought to give incorrect instructions to immune cells, leading to the production of the harmful antibodies.
- Genetic Factors: There may be a genetic predisposition to developing MG, as it sometimes occurs in more than one family member. However, the precise genetic factors involved are still being researched.
Types of Myasthenia Gravis
MG can be classified into different types based on the age of onset, distribution of muscle weakness, and the presence of specific antibodies. The main types include:
- Ocular Myasthenia Gravis:
- This type affects only the eye muscles, leading to symptoms such as ptosis and diplopia. It does not progress to generalized MG in many patients.
- Generalized Myasthenia Gravis:
- In this type, multiple muscle groups are affected, including ocular, bulbar (facial and throat), limb, and respiratory muscles.
- Congenital Myasthenia Gravis:
- This rare type is present at birth and is caused by genetic mutations affecting the neuromuscular junction.
- Juvenile Myasthenia Gravis:
- Occurring in children and adolescents, this type often involves the same symptoms as generalized MG.
- Seronegative Myasthenia Gravis:
- Patients with this type do not have detectable levels of the common antibodies (anti-acetylcholine receptor or anti-MuSK antibodies) associated with MG but still exhibit the typical symptoms.
Diagnosis of Myasthenia Gravis
Diagnosing MG involves a combination of clinical evaluation, laboratory tests, and imaging studies. Common diagnostic methods include:
- Physical Examination and Medical History: A detailed history and examination can reveal characteristic muscle weakness patterns.
- Edrophonium Test: Injection of edrophonium chloride, a drug that temporarily increases acetylcholine levels, can improve muscle strength in MG patients, aiding diagnosis.
- Blood Tests: Detection of specific antibodies (anti-acetylcholine receptor or anti-MuSK antibodies) helps confirm the diagnosis.
- Electromyography (EMG): This test measures electrical activity in muscles and can detect impaired nerve-to-muscle transmission.
- Imaging Studies: CT or MRI scans can identify thymus gland abnormalities, such as thymomas.
Treatment of Myasthenia Gravis
There is no cure for MG, but various treatments can help manage symptoms and improve quality of life. The primary treatment options include:
- Medications:
- Anticholinesterase Inhibitors: Drugs like pyridostigmine (Mestinon) increase acetylcholine levels at the neuromuscular junction, enhancing muscle contraction.
- Immunosuppressants: Medications such as prednisone, azathioprine, and mycophenolate mofetil suppress the immune response to reduce antibody production.
- Intravenous Immunoglobulin (IVIG): IVIG therapy provides normal antibodies that modify the immune response.
- Plasmapheresis: This procedure filters the blood to remove harmful antibodies, providing temporary relief from symptoms.
- Thymectomy: Surgical removal of the thymus gland can improve symptoms, especially in patients with thymomas or generalized MG.
- Lifestyle and Supportive Measures:
- Physical Therapy: Helps maintain muscle strength and function.
- Speech and Occupational Therapy: Assists with communication and daily activities.
- Respiratory Support: In severe cases, mechanical ventilation may be required during a myasthenic crisis.
- Experimental Treatments:
- Research is ongoing into new therapies, such as monoclonal antibodies (e.g., eculizumab) and other immunomodulatory drugs, which may offer additional treatment options in the future.
Conclusion
Myasthenia Gravis is a complex autoimmune disorder that significantly impacts the lives of those affected. Early diagnosis and comprehensive treatment are essential for managing symptoms and improving the quality of life. With ongoing research and advancements in medical treatments, there is hope for even better management strategies and outcomes for individuals with MG. Understanding the symptoms, causes, types, and treatment options enables patients, caregivers, and healthcare professionals to work together effectively in managing this challenging condition.