Black Fungal Infection: Understanding Mucormycosis

What Is Black Fungal Infection
Black fungal infection, medically referred to as Mucormycosis, is a rare yet serious infection caused by a group of molds known as mucormycetes. These molds naturally exist in the environment, particularly in soil and decaying organic matter like leaves, compost, and rotting wood. What makes Mucormycosis noteworthy is its rapid impact on individuals with compromised immune systems.
Mucormycosis
Mucormycosis primarily attacks individuals with weakened health defenses, manifesting in various forms depending on where the fungus is growing within the body. Commonly, it affects the sinuses or lungs after inhaling fungal spores from the air. This can lead to rhinocerebral (sinus and brain) mucormycosis, pulmonary (lung) mucormycosis, and in some severe cases, can disseminate to other parts of the body. Unlike common molds, mucormycetes can be life-threatening, especially in diabetics or people undergoing immune-suppressing treatments.
Types of Black fungus disease Mucormycosis
Black fungus disease, or mucormycosis, can be categorized into several types based on the area of the body it affects:
- Rhinocerebral Mucormycosis: Affects the sinuses and brain, commonly seen in diabetic patients.
- Pulmonary Mucormycosis: Involves the lungs, often affecting individuals with weakened immune systems.
- Cutaneous Mucormycosis: Appears on the skin, usually due to trauma or skin injury.
- Gastrointestinal Mucormycosis: Affects the stomach and intestines, more common in premature infants and malnourished individuals.
- Disseminated Mucormycosis: Spreads to multiple organs, including the brain, spleen, and heart.
- Renal Mucormycosis: Involves the kidneys, a rare form often diagnosed post-mortem.
- Oral Mucormycosis: Affects the oral cavity, including the palate and maxilla, frequently in patients with hematological malignancies.
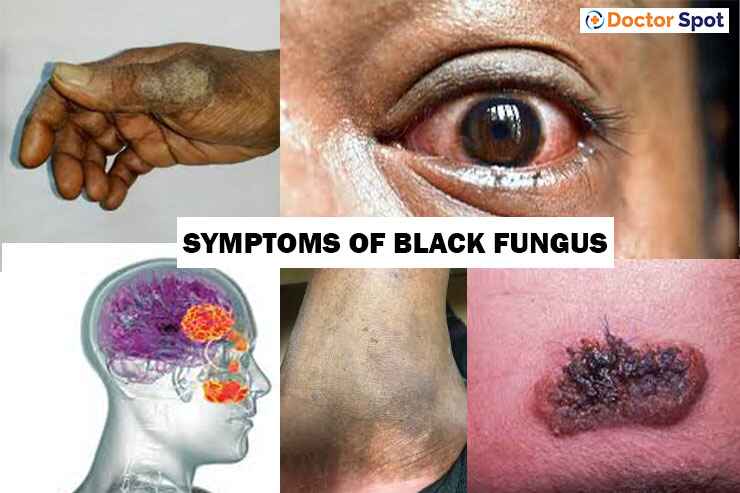
Symptoms of Mucormycosis
The symptoms of Mucormycosis vary greatly depending on the affected area:
- Rhinocerebral Mucormycosis: Facial swelling, congestion, nasal discharge (which may be black or bloody), and severe headache.
- Pulmonary Mucormycosis: Fever, cough, chest pain, and shortness of breath.
- Cutaneous Mucormycosis: Blackened skin tissue, pain, redness, swelling, and tenderness over the affected area.
It’s crucial to recognize these symptoms early as Mucormycosis requires prompt medical attention due to its aggressive nature.
Diagnosis and Treatment
Diagnosing Mucormycosis typically involves tissue biopsy, which then undergoes a fungal culture in a lab. Imaging tests such as CT scans or MRIs can also be employed to assess the spread within the body.
Treatment is equally aggressive, involving antifungal medications like Amphotericin B, Posaconazole, or Isavuconazole. In severe cases, surgical removal of the affected tissue might be necessary to prevent the infection from spreading further. Early diagnosis and treatment significantly improve outcomes.
Risk Factors of Mucormycosis
The following conditions or situations can increase the risk of developing Mucormycosis:
- Diabetes, particularly when poorly controlled
- Use of corticosteroids which suppress the immune system
- Undergoing organ or stem-cell transplantation
- Iron overload which provides an environment conducive to fungal growth
- Neutropenia (low levels of white blood cells)
Prevention of Mucormycosis
Preventive measures for Mucormycosis focus on limiting exposure to areas where the mold may thrive:
- Avoiding areas with excessive dust and stored contaminated items.
- Wearing masks and protective clothing when working with soil, moss or manure.
- Regular maintenance of hygiene especially in hospital settings and around immuno-compromised individuals.
When to Visit a Doctor for Black Fungal Infection
Immediate medical attention should be sought if symptoms suggestive of Mucormycosis appear, particularly in individuals with risk factors. Early detection and management can be the difference between recovery and severe health outcomes.
FAQs
Q: Can Mucormycosis spread between people?
A: No, Mucormycosis is not contagious and cannot be transmitted between individuals.
Q: Is there a vaccine for Mucormycosis?
A: Currently, there is no vaccine available that protects against Mucormycosis. The best prevention involves managing underlying health conditions and avoidance of high-risk environments.
Q: Are there any new treatments being developed?
A: Research is ongoing to develop more effective treatments for fungal infections including Mucormycosis. Advances in antifungal therapies and improved diagnostic tools are being studied.
By understanding what Mucormycosis is, recognizing the symptoms, and knowing when to seek medical help, individuals can significantly mitigate the risks posed by this dangerous infection. Always consult healthcare providers for a definitive diagnosis and appropriate treatment plan tailored to individual health conditions.