Follicle Size (Egg size) and Ovulation: A Day-by-Day Guide for IUI
Intrauterine insemination (IUI) is one of the most commonly performed assisted reproductive techniques for couples dealing with infertility.
One of the key factors in the success of IUI is monitoring the growth of ovarian follicles to determine the ideal time for insemination. The size of the follicle plays a major role in predicting ovulation, ensuring sperm is placed at the most fertile window.
This guide will walk you through day-by-day follicle development, the role of follicle size in ovulation, and how doctors decide the right time for IUI.
1. Understanding Follicles and Their Role in Ovulation
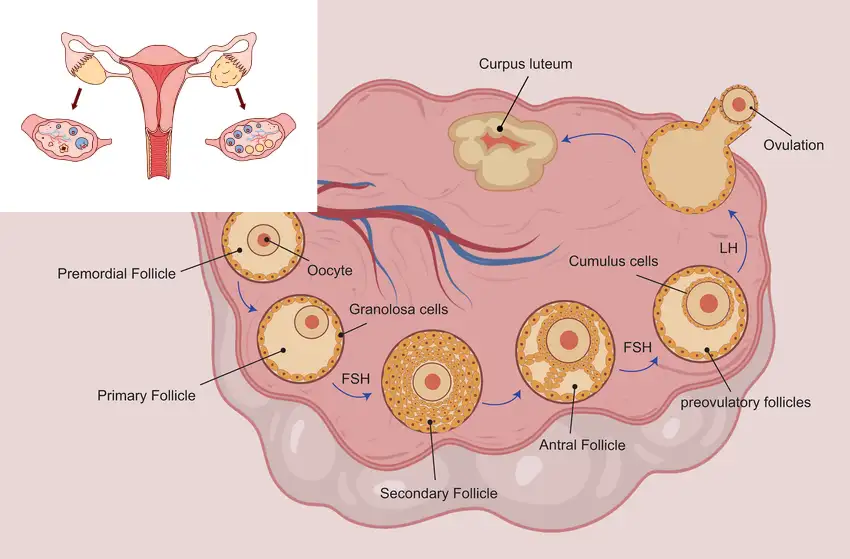
Before diving into the daily progression, it’s important to understand what follicles are.
-
Follicles are small sacs inside the ovaries that contain immature eggs (oocytes).
-
Every month, several follicles start to grow, but usually only one becomes dominant and reaches maturity.
-
Ovulation occurs when the mature follicle ruptures and releases the egg into the fallopian tube.
-
Follicle size is monitored via transvaginal ultrasound scans.
Normal Follicle Size Milestones:
| Stage | Follicle Size (mm) | Description |
|---|---|---|
| Early development | 2–5 mm | Resting follicles |
| Growing phase | 6–10 mm | Several follicles grow |
| Pre-ovulatory | 16–22 mm | Dominant follicle emerges |
| Ovulation-ready | 18–24 mm | Ideal size for egg release |
2. Why Follicle Size Matters in IUI
-
Predicting ovulation: Follicles grow at an average rate of 1–2 mm per day after stimulation.
-
Scheduling IUI: The insemination is timed just before or on the day of ovulation.
-
Preventing early or late insemination: Too early means the egg isn’t ready; too late means the egg may no longer be viable.
-
Trigger shot timing: An hCG injection may be given when the follicle reaches 18–20 mm to induce ovulation.
3. Day-by-Day Follicle Growth in IUI Cycles
The exact timeline varies depending on:
-
Whether the cycle is natural or medicated
-
The type of medication used (Clomiphene, Letrozole, or Gonadotropins)
-
The woman’s ovarian reserve and age
Below is a generalized day-by-day guide for a medicated IUI cycle:
Day 1–3 Follicle size / Egg size : Menstrual Phase & Baseline Scan
-
The cycle starts on Day 1 of the period.
-
On Day 2 or 3, a baseline ultrasound scan is performed.
-
The scan checks for:
-
Absence of cysts
-
Baseline follicle count (Antral Follicle Count – AFC)
-
Uterine lining thickness (should be thin, ~2–4 mm)
-
-
Medications to stimulate ovulation are started, such as:
-
Clomiphene Citrate (CC) – 50–150 mg/day for 5 days
-
Letrozole – 2.5–5 mg/day for 5 days
-
Gonadotropin injections – FSH or HMG
-
Day 5–7 follicle size / Egg size : Early Follicular Growth
-
Small follicles begin to grow under the effect of medication.
-
Follicle size: 5–8 mm
-
Uterine lining: 3–5 mm
-
No dominant follicle yet; multiple follicles may be developing.
Tips for Patients:
-
Continue medications as prescribed.
-
Maintain hydration and a balanced diet.
-
Avoid self-checking for ovulation at this stage—it’s too early.
Day 8–10 follicle size / Egg size: Mid-Follicular Phase
-
The first monitoring scan is often scheduled on Day 8 or 9.
-
Follicle size: 10–14 mm
-
The doctor identifies the dominant follicle—the one growing faster than the others.
-
Follicles grow at ~1.5–2 mm per day after this stage.
-
Uterine lining should be at least 6–8 mm and triple-layered for better chances of implantation.
If Follicles Are Slow:
-
Dosage of gonadotropins may be increased.
-
The next scan is scheduled in 2 days.
Day 11–13: Pre-Ovulatory Phase
-
Follicle size: 16–20 mm
-
This is the critical window for deciding IUI timing.
-
If the follicle is ≥18 mm, a trigger shot (hCG 5,000–10,000 IU) is usually administered to induce ovulation within 36–40 hours.
-
Uterine lining ideally 8–12 mm.
Typical Scenario:
-
Day 11: Follicle at 17 mm → Trigger shot given.
-
Day 13: IUI performed.
Day 14–16: Ovulation & IUI
-
Ovulation occurs ~36 hours after the trigger shot.
-
Follicle size at rupture: 22–24 mm (appears collapsed on scan post-ovulation).
-
IUI is done:
-
Single IUI: Performed ~36 hours after trigger.
-
Double IUI: Performed at 24 hours and again at 48 hours post-trigger.
-
Note:
-
In natural cycles without a trigger shot, ovulation is timed based on LH surge detection via blood/urine tests.
4. Example Timeline for a Medicated IUI Cycle
| Cycle Day | Follicle Size | Uterine Lining | Action |
|---|---|---|---|
| Day 2 | 2–5 mm | 2–4 mm | Baseline scan, start meds |
| Day 8 | 10–12 mm | 6 mm | First monitoring scan |
| Day 10 | 14–16 mm | 7–8 mm | Continue meds |
| Day 12 | 18–20 mm | 8–10 mm | Trigger shot given |
| Day 14 | 22–24 mm (rupture) | 9–12 mm | IUI performed |
5. Factors That Can Affect Follicle Growth
-
Age – Ovarian reserve decreases with age, affecting follicle growth rate.
-
PCOS – May cause multiple small follicles that fail to mature.
-
Endometriosis – May impact follicle quality.
-
Medication response – Some women may require higher doses.
-
Lifestyle – Stress, poor nutrition, and smoking can slow growth.
6. How Doctors Decide the Right Follicle Size for Trigger
-
Most doctors give a trigger when at least one follicle reaches 18–20 mm.
-
Too small (<16 mm) – Egg may be immature.
-
Too large (>24 mm) – Risk that the egg is post-mature and less viable.
-
For women with multiple mature follicles, doctors discuss the risk of twins/multiples before proceeding.
7. Tips for Maximizing IUI Success
-
Follow scan schedules strictly – Even 1-day delay can miss the ovulation window.
-
Avoid excessive exercise during stimulation – Can affect blood flow to ovaries.
-
Maintain healthy weight – Both underweight and overweight women may have slower follicle growth.
-
Track symptoms – Mild bloating or pelvic discomfort can indicate follicle growth.
-
Discuss luteal phase support – Progesterone supplementation may be given after IUI.
8. FAQs on Follicle Size and IUI
Q1: Can a 17 mm follicle release a mature egg?
A: Yes, but the optimal maturity is usually at 18–20 mm.
Q2: How many follicles are ideal for IUI?
A: 1–2 dominant follicles; more than 3 increases risk of multiples.
Q3: Can follicles stop growing?
A: Yes, due to poor medication response, hormonal imbalance, or ovarian aging.
Q4: What if no follicle reaches maturity?
A: The cycle may be canceled or converted to IVF for better control.
Conclusion
Follicle size monitoring is one of the most critical aspects of IUI treatment. Understanding day-by-day growth helps both doctors and patients plan insemination at the most fertile moment, improving the chances of pregnancy.
With careful ultrasound tracking, hormonal support, and proper timing, IUI can be an effective and affordable fertility treatment for many couples.